Why Candida albicans Septicemia Models Have Become Essential in Infectious Disease Research
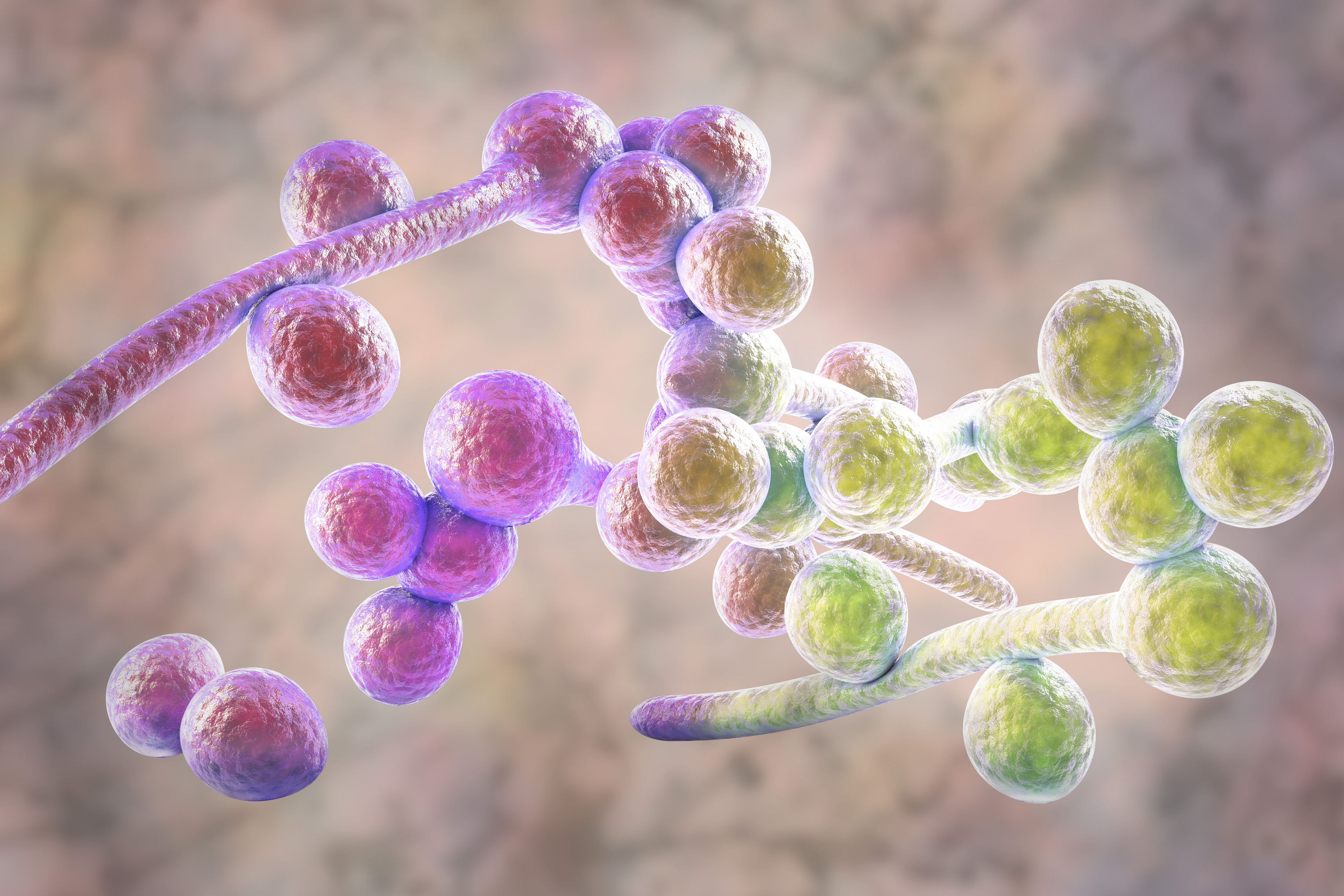
In the ongoing struggle against infectious diseases, while viruses and bacteria often take center stage, invasive fungal infections represent a silent but growing threat to global health. The emergence of antifungal-resistant strains and the high mortality rates associated with systemic candidiasis make the development of relevant preclinical models critical.
Animal models, particularly murine models, have fundamentally transformed the way we investigate fungal pathogenesis and host responses. Today, the Candida albicans septicemia model has become an essential tool, enabling scientists to explore the intricate mechanisms of host-pathogen interaction in vivo with the depth and fidelity required to develop new therapies.
Overcoming Challenges in Antifungal Research
One of the central challenges in developing new antifungals lies in the complexity of human infection. Patients suffering from invasive candidiasis often present with comorbidities or immunosuppression that complicate the clinical picture. Furthermore, the limited number of available antifungal classes and the rise of resistance necessitate models capable of accurately predicting the efficacy of new molecules.
In vitro models, while useful, cannot reproduce the dynamics of systemic dissemination or the host's complex immune response. This is where the murine model of systemic candidiasis proves invaluable, offering a robust platform to evaluate therapeutic efficacy and understand virulence.
The Candida albicans Septicemia Model
Among the fungal models available today, the septicemia model of Candida albicans via intravenous injection is considered the "Gold Standard" for antifungal drug evaluation.
This model typically involves the injection of a calibrated inoculum of C. albicans yeast into the mouse tail vein. The pathogen then rapidly disseminates through the bloodstream to reach deep organs, primarily targeting the kidneys, as well as the brain and liver.
In the context of infectious disease research, this model offers several decisive advantages:
- High Reproducibility: The infection follows a well-characterized kinetic, allowing for robust and comparable statistical data.
- Clinical Mimicry: It recapitulates key features of human fungal sepsis, including systemic inflammatory response, weight loss, and progressive renal failure.
- Precise Therapeutic Assessment: It allows for the testing of new antifungal molecules and the determination of optimal dosing regimens.
- Virulence Studies: This model is ideal for comparing the pathogenicity of different clinical strains or genetic mutants (e.g., strains unable to form hyphae).
- Regulatory requirement: Agencies such as the FDA or EMA almost systematically request data from this model before authorizing clinical trials.
Broader Applications in Infectious Disease
Beyond simple drug screening, the C. albicans septicemia model is instrumental in modeling:
- Immunomodulation: Understanding how the innate immune system (neutrophils, macrophages) responds to the fungal invader and testing adjuvant immunotherapies.
- Resistance Mechanisms: Studying in vivo therapeutic failure due to azole- or echinocandin-resistant strains.
Vaccine Development: Assessing the ability of vaccine candidates to protect against lethal infection.
Vibiosphen’s Approach
At Vibiosphen, we understand that the translational value of a model is paramount. By integrating the Candida albicans septicemia model into our platform, we support the design, execution, and interpretation of rigorous preclinical studies.
Our expertise allows us to adapt this model (through validation of new strains) to specific needs: using specific clinical strains, modifying the host's immune status (immunosuppressed models), or analyzing specific biomarkers (tissue fungal burden, cytokine profiling).
Limitations and Future Perspectives
While robust and widely used, this model presents certain limitations. The intravenous route of inoculation bypasses natural mucosal barriers (such as the gut and skin) and, consequently, the mucosal immune responses normally involved in this type of infection.
It remains the reference model for assessing antifungal efficacy, yet it does not replicate the full complexity of epithelial barriers. For this reason, Vibiosphen has complemented it with a translocation model, which we will describe in a forthcoming article.
Ongoing advances such as humanized mouse systems, bacteria–fungi co-infection models, and organ-on-chip technologies, continue to enhance the physiological relevance of infection modeling.
Candida albicans septicemia models are redefining what is possible in the fight against invasive mycoses. As fungal threats evolve, the need for relevant, ethical, and powerful preclinical models has never been more urgent to accelerate the discovery of the next generation of antifungals.
Catégories
Pagination
- Page précédente
- Page 2
Archives
- janvier 2026 (2)
- octobre 2025 (1)
- juillet 2025 (1)
- juin 2025 (3)
- mai 2025 (1)
- mars 2025 (1)
- mai 2024 (1)
- avril 2024 (2)
- septembre 2023 (1)
- août 2023 (1)
- mai 2023 (1)
- avril 2023 (2)
- février 2023 (1)
- décembre 2022 (1)
- octobre 2022 (1)
- juin 2022 (1)
- mai 2022 (3)
- avril 2022 (1)
- février 2022 (2)
- janvier 2022 (3)
- décembre 2021 (2)
- novembre 2021 (1)