The cutaneous microbiome: a lever in acne treatment

Vulgar acne is a common inflammatory skin disorder of the pilosebaceous unit. It’s characterized by seborrhea and abnormalities in follicular keratinization (1). Today, acne is recognized as a multifactorial condition (hormonal factors, seborrhea, cutaneous inflammation, etc), with a high prevalence among young adults (16-24 years old) (2).
Beyond its visible manifestations (pimples, blackheads, cysts), acne can profoundly affect self-esteem and lead to significant social stigma (3).
Among the various factors involved in acne, one actor is attracting increasing interest: skin microbiota. It has been scientifically demonstrated that microbiota plays a role in acne pathogenesis, primarily through a state of imbalance (dysbiosis) (1-5). Understanding its involvement opens the door to new perspectives for the treatment and prevention of acne.
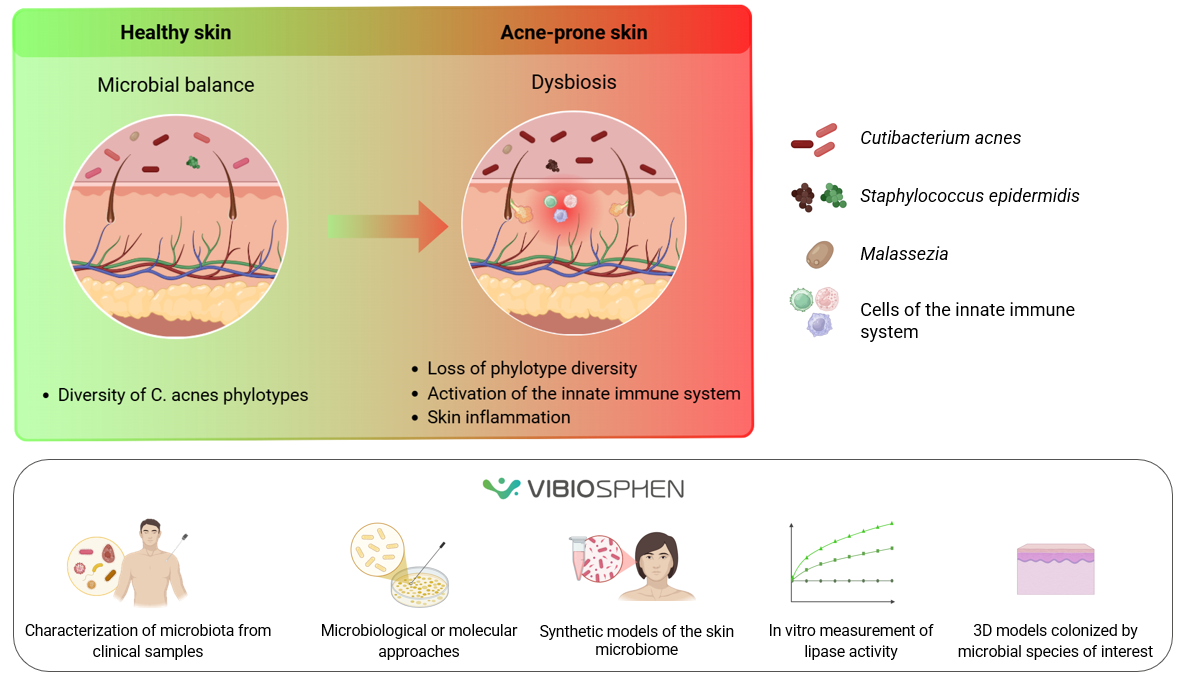
Consequences of dysbiosis in acne:
Comparisons of different bacterial populations between healthy and acne-affected skin highlight the role of certain strains.
The central role of Cutibacterium acnes (C. acnes):
C. acnes, a major commensal bacterium of the skin microbiota, contributes to the pathogenesis of acne (3). Recent skin microbiome characterization of C. acnes strain populations, from acne patients and individuals with healthy skin, demonstrates the importance of C. acnes genetic elements as a major acne determinant (1,3,4,5). Indeed, the development of acne is strongly associated with specific strains and phylotypes of C. acnes (4).
Staphylococcus epidermidis (S. epidermidis):
Moreover, according to recent studies, the interaction between S. epidermidis and C. acnes plays a key role in skin homeostasis. Indeed, S. epidermidis, through the fermentation of glycerol into succinic acid, can control the proliferation of C. acnes and reduce the associated cutaneous inflammation. Conversely, C. acnes inhibits the growth of S. epidermidis by maintaining an acidic environment. However, during dysbiosis, as observed in acne, the abundance of the different C. acnes phylotypes is altered, contributing to microbiota imbalance and cutaneous inflammation (1).
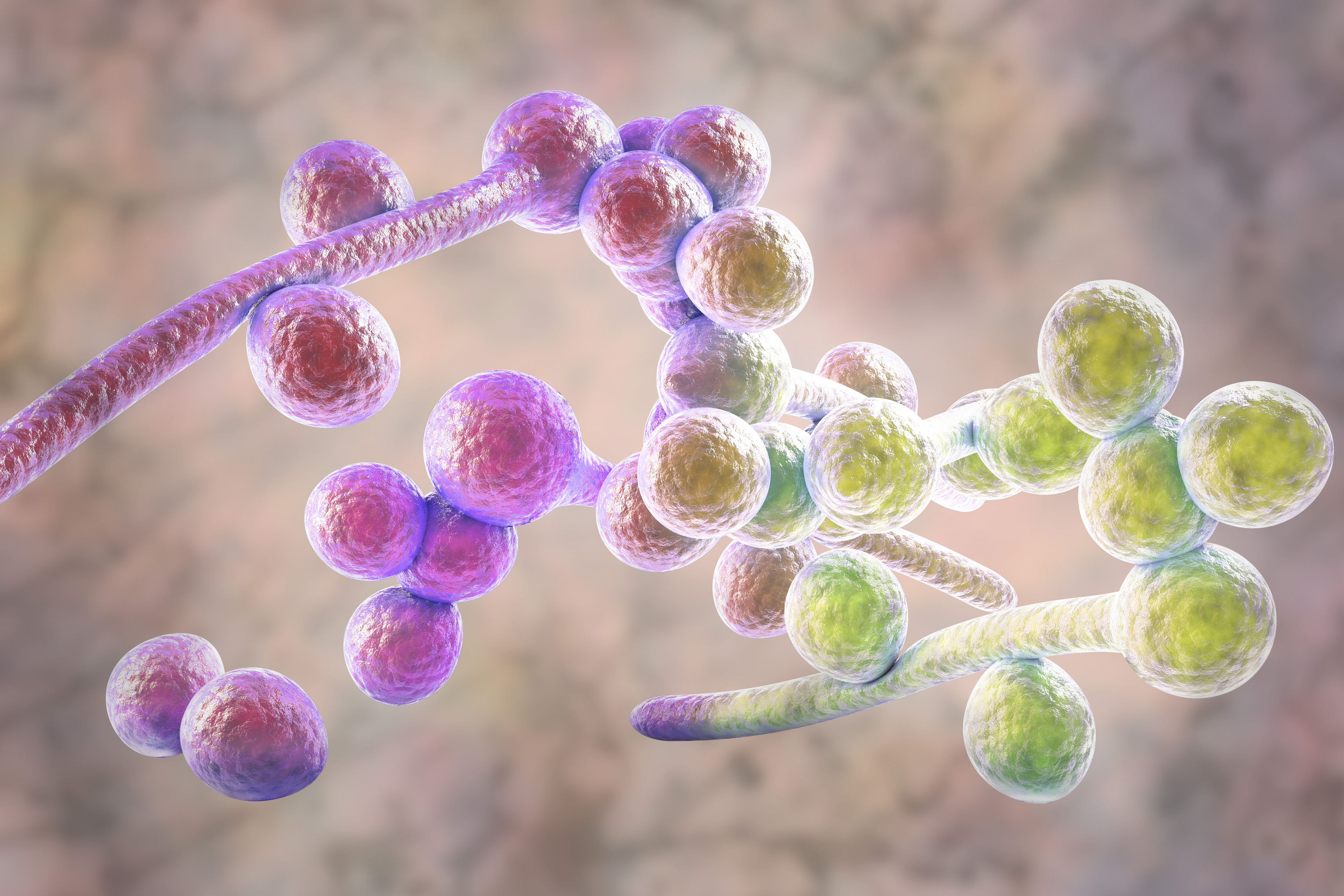
Role of Malassezia:
Malassezia, the most abundant fungus on the skin, may contribute to refractory acne. Although its exact role in the pathophysiology of acne remains to be elucidated, it may be involved in increased cutaneous inflammation (1).
It’s also important to note that the bacterial interactions involved in acne are not limited to the skin: individuals with acne also exhibit differences in the gut microbiota (5).
These studies, together with the growing interest in the microbiota, pave the way for targeted strategies aimed at preventing or treating dysbiosis.
At Vibiosphen, we offer solutions tailored to our clients’ needs:
Support for microbiota characterization from clinical samples
Microbiological or molecular approaches, targeted or global
Development of synthetic skin microbiome models
In vitro measurement of lipase activity
3D models, including human skin explants or reconstructed human epidermis colonized with microbial species of interest
Thus, we contribute to a better understanding of microbial interactions and to the assessment of the impact of new formulations on the skin microbiome.
Sources:
- Dréno B, Dagnelie MA, Khammari A, et al. The skin microbiome: a new actor in inflammatory acne. Am J Clin Dermatol. 2020;21(Suppl 1):18–24. doi:10.1007/s40257-020-00531-1
- Saurat JH, Halioua B, Baissac C, et al. Epidemiology of acne and rosacea: a worldwide global study. J Am Acad Dermatol. 2024;90(5):1016–1018. doi:10.1016/j.jaad.2023.12.038.
- Cavallo I, Sivori F, Truglio M, et al. Skin dysbiosis and Cutibacterium acnes biofilm in inflammatory acne lesions of adolescents. Sci Rep. 2022;12:21104. doi:10.1038/s41598-022-25436-3.
- Hajam IA, Katiki M, McNally R, et al. Functional divergence of a bacterial enzyme promotes healthy or acneic skin. Nat Commun. 2023;14:8061. Doi:10.1038/s41467-023-43833-8.
- Huang C, Zhuo F, Han B, et al. The updates and implications of cutaneous microbiota in acne. Cell Biosci. 2023;13:113. doi:10.1186/s13578-023-01072-w.
Catégories
Pagination
- Page 1
- Page suivante
Archives
- février 2026 (2)
- janvier 2026 (2)
- octobre 2025 (1)
- juillet 2025 (1)
- juin 2025 (3)
- mai 2025 (1)
- mars 2025 (1)
- mai 2024 (1)
- avril 2024 (2)
- septembre 2023 (1)
- août 2023 (1)
- mai 2023 (1)
- avril 2023 (2)
- février 2023 (1)
- décembre 2022 (1)
- octobre 2022 (1)
- juin 2022 (1)
- mai 2022 (3)
- avril 2022 (1)
- février 2022 (2)
- janvier 2022 (3)
- décembre 2021 (2)
- novembre 2021 (1)